Confidently Know When You Need Root Canal Treatment – 8 Basic Symptoms
Maintaining good dental health is essential for overall well-being, yet many people overlook early warning signs of dental problems. One common procedure that often causes concern is a root canal. If you’re experiencing dental discomfort, you might wonder, do I need root canal treatment? Recognizing the key symptoms can help you take action early and prevent more serious issues. In this guide, we’ll discuss how to confidently identify if you need a root canal by understanding the main warning signs.

Table of Contents
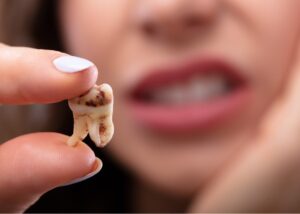
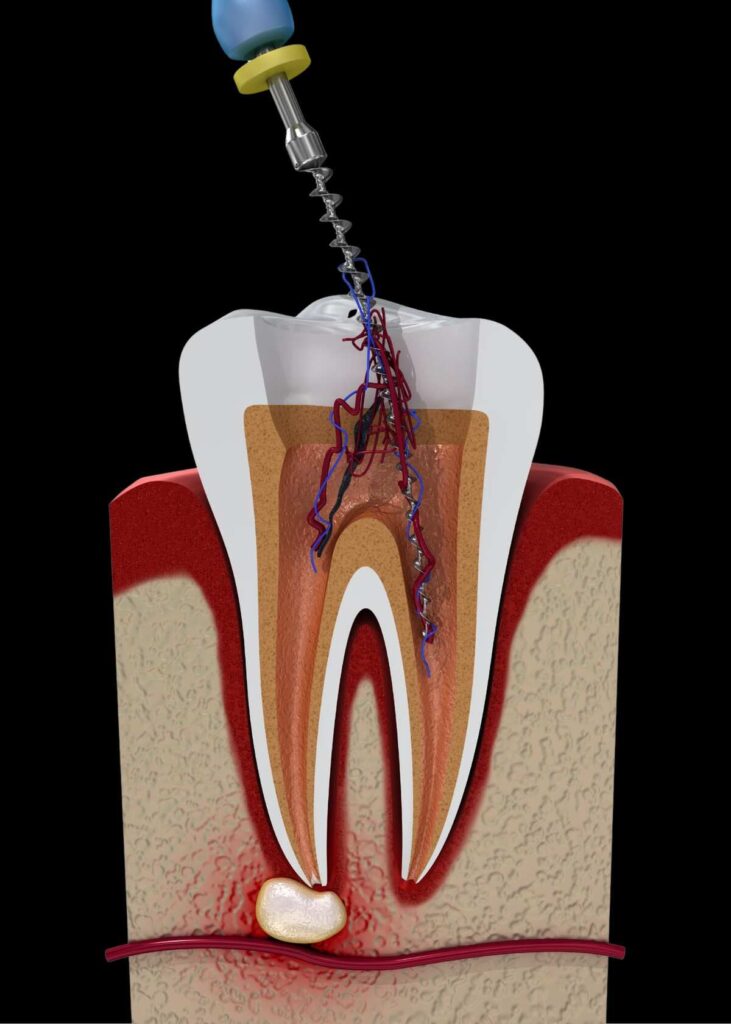
What Is a Root Canal Treatment?
Root canal treatment, also known as endodontic therapy, is a procedure aimed at saving a tooth that has become infected or severely decayed. When bacteria invade the pulp (the soft tissue inside your tooth that contains nerves and blood vessels), it can cause intense pain and infection. The treatment involves removing the infected tissue, thoroughly disinfecting the canal system, and sealing it to prevent further infection. Though it’s often misunderstood, a root canal can preserve your natural tooth and restore normal function.
Why Recognizing the Need for a Root Canal Is Crucial
Delaying treatment when you need a root canal can lead to serious complications, such as abscess formation, bone loss, or even tooth loss. Early detection ensures less invasive procedures, less discomfort, and a higher chance of saving your natural tooth. So, how can you tell if you need a root canal? Let’s look at the key symptoms that indicate you should see a dentist promptly.
Key Symptoms That Signal You Might Need a Root Canal
1. Ongoing Tooth Pain
A consistent or recurring toothache is often the hallmark sign that you require root canal treatment. Unlike occasional discomfort, a tooth requiring treatment often causes continuous, throbbing pain that worsens with pressure or exposure to hot and cold stimuli. This pain can be dull or sharp and may linger even after the trigger has been removed.
Why it happens: Infection or inflammation in the pulp irritates the nerve endings inside the tooth, leading to persistent pain.
What to do: If your toothache persists for more than a couple of days, it’s important to consult your dentist without delay.
2. Increased Sensitivity to Hot and Cold
Heightened sensitivity when consuming hot or cold foods and beverages is another warning sign. If the sensitivity lasts long after the stimulus is gone, it could indicate nerve damage or pulp infection.
Why it occurs: Damage to the pulp makes the nerve endings more reactive, leading to increased sensitivity.
What to do: Avoid extreme temperatures and seek dental advice to determine if treatment is needed.
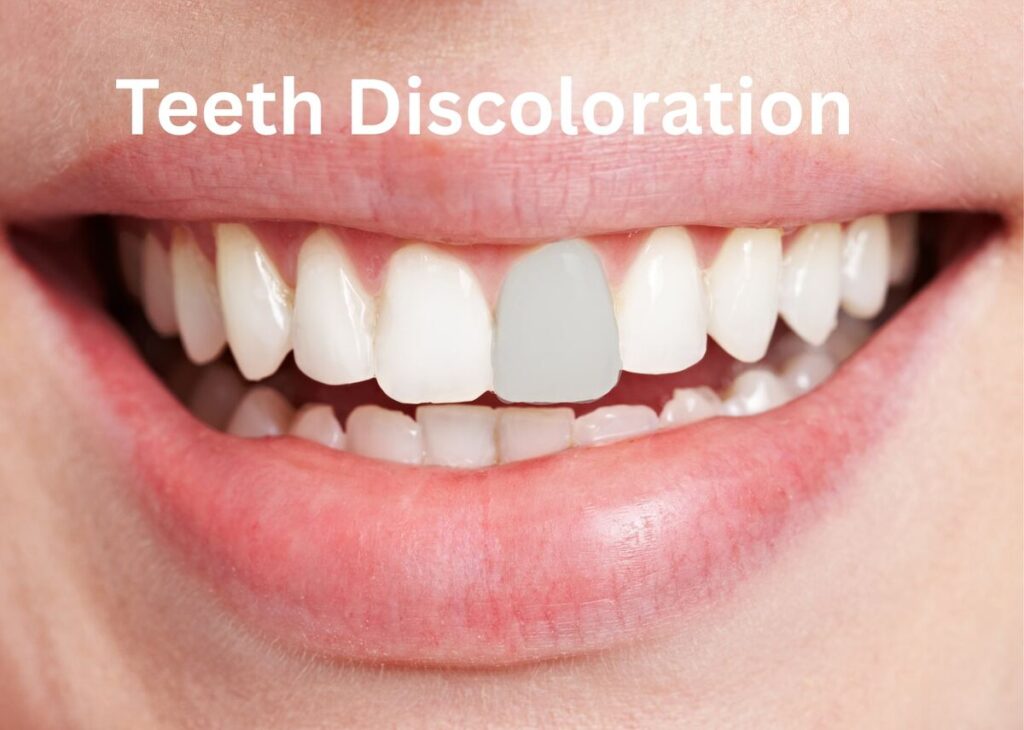
3. Discoloration of the Tooth
A tooth that appears darker or develops a different shade than neighboring teeth often signals pulp necrosis (death of the pulp tissue). This change in color results from internal bleeding or tissue necrosis.
Why it happens: When the pulp tissue dies, the tooth can turn gray, brown, or black.
What to do: Discoloration should be examined by a dental professional to decide if root canal treatment is necessary.
4. Swelling and Tenderness
Swelling or tenderness in the gums or face near the affected tooth is a clear sign of infection. You may notice a tender or swollen gum area near the problematic tooth, sometimes accompanied by a pus-filled abscess.
Why it happens: Infection from the pulp can spread to surrounding tissues, causing inflammation and swelling.
What to do: Swelling requires immediate evaluation by your dentist to prevent the infection from worsening.
5. Pain When Chewing or Biting
Pain while chewing or applying pressure on a specific tooth is often a sign of pulp inflammation or infection. This discomfort may be sharp or dull and typically worsens with continued biting.
Why it occurs: Infection or inflammation weakens the tooth’s ability to withstand biting forces.
What to do: Avoid chewing on that side and seek dental care promptly.
6. Abscess or Pus Drainage
A visible bump or abscess on the gums near the affected tooth that releases pus is a significant sign of infection. This indicates a severe infection that often requires root canal treatment to eliminate the infection and preserve the tooth.
Why it occurs: The body forms an abscess to contain the infection, leading to pus accumulation.
What to do: Seek immediate dental attention to drain the abscess and treat the underlying problem.
7. Bad Taste or Persistent Foul Odor
An unpleasant taste or foul smell in your mouth, especially near a specific tooth, can indicate ongoing infection or decay inside the tooth.
Why it happens: Bacterial activity within the infected pulp produces foul substances that can be tasted or smelled.
What to do: If these symptoms persist, consult your dentist for assessment and treatment.

8. Looseness of the Tooth
In cases of severe infection or abscess, the supporting structures of the tooth may weaken, leading to a sensation of looseness.
Why it occurs: Infection destroys surrounding bone and tissues holding the tooth in place.
Immediate action: A loose tooth requires quick evaluation to prevent eventual loss.
Additional Signs That May Indicate the Need for Root Canal
- Recurrent decay or deep cavities – that expose the pulp to bacteria.
- Cracks or fractures – extending into the pulp chamber.
- Persistent pain – after dental restorations, such as fillings or crowns.
- Radiographic evidence – showing dark areas around the root tips, indicating infection or abscess.
- Persistent pain after dental procedures: Ongoing discomfort after fillings or crowns may signal unresolved pulp issues.
When to Visit Your Dentist
If you are having any of these symptoms, schedule an appointment with your dentist as soon as possible. Early diagnosis and treatment can prevent the infection from spreading and reduce the need for more invasive procedures.
Remember: Do not ignore persistent or worsening dental pain. While some discomfort might resolve naturally, ongoing symptoms are a clear signal that professional evaluation is necessary.
How Dentists Confirm You Need a Root Canal
Dentists use a combination of clinical examinations, patient history, and diagnostic tools to determine if you need a root canal:
- X-rays: These reveal the extent of decay, infection, or abscesses.
- Pulp testing: Thermal and electric tests assess nerve vitality.
- Visual inspection: Checking for swelling, discoloration, and gum health.
Based on these assessments, your dentist will recommend the most appropriate treatment plan.
Final Thoughts: Act Quickly and Confidently
Understanding the key symptoms that indicate you might need a root canal empowers you to seek timely dental care. Persistent toothache, sensitivity, swelling, discoloration, and pain when chewing are all signs that should not be ignored. Early intervention not only relieves pain but also saves your natural tooth and prevents more serious health issues.
If you notice any of these symptoms, contact Sparsh Dental Clinic in Bilaspur or Dentist near you. Remember, early diagnosis and treatment can make all the difference in maintaining your dental health and keeping your smile bright and healthy.
Take charge of your dental health today—recognize the signs, seek professional advice, and enjoy a pain-free, healthy smile!
Visit Sparsh Dental Clinic for expert care and personalized treatment plans.